Diagnosis
Diagnosis of iron deficiency involves careful history taking and physical examination, which are essential in identifying risk factors and possible etiology, guiding laboratory testing, and identifying the underlying cause of the iron deficiency.

Laboratory Testing
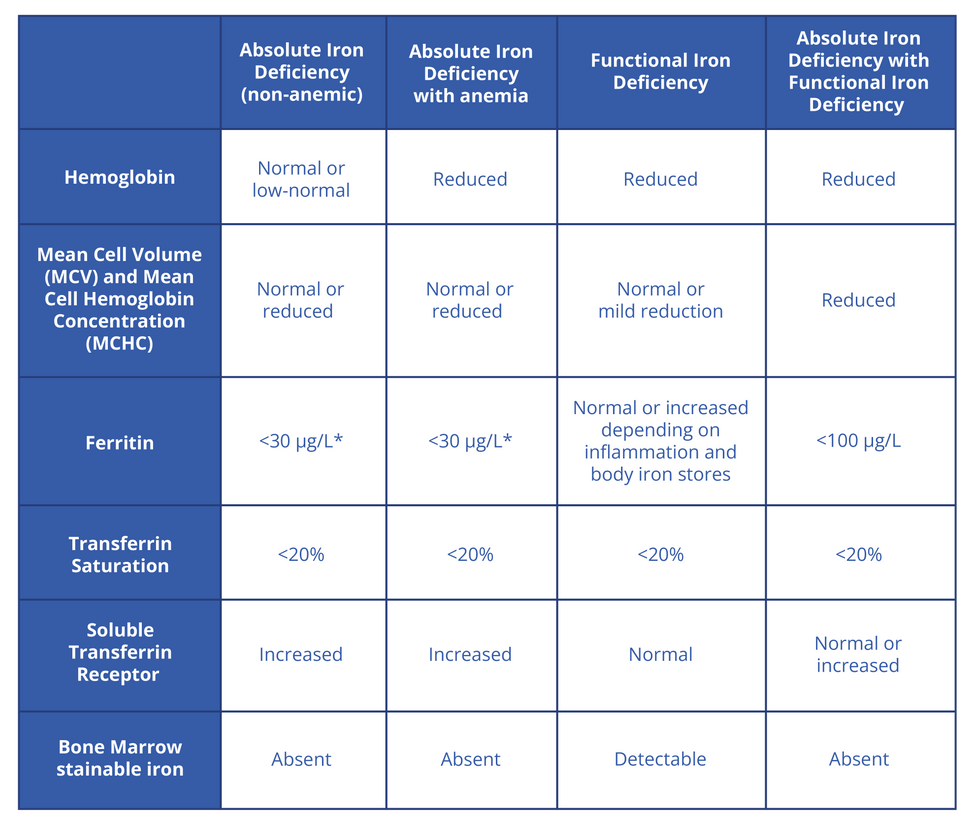
Laboratory Findings at Different Stages of Iron Deficiency
*A ferritin level below 30 is considered as the threshold diagnose iron deficiency, however there is recent evidence suggesting that a level below 50 ug/L is in keeping with iron deficiency, as it is associated with fatigue, which improves with treatment. (1) (2)

Complete Blood Count (CBC)
A complete blood count (CBC) may show:
Anemia
Reduced mean cell hemoglobin (MCHC) and mean cell volume (MCV) These are sensitive measures, however they become abnormal only in longstanding iron deficiency, and reduced MCHC and MCV may also be decreased in hemoglobinopathies and sideroblastic anemia. MCV may be normal in ID in combined nutrient deficiency, such coexisting vitamin B12 deficiency. In one study, approximately 25% of patients with iron deficiency were found to have a normal or elevated MCV. [3]
Elevated red cell distribution width (RDW)
Elevated platelet count in some cases

Peripheral Blood Smear
A peripheral blood smear may show:
Microcytic hypochromic red blood cells
Anisocytosis (variation in the shape of the cells)
Poikilocytosis (variation in the size of the cells)
Less common findings include Elliptocytes (elliptical shaped RBC) Polychromasia (variation in the color of the RBC, indicating presence of reticulocyte) Basophilic stippling

Ferritin
Ferritin is a protein that sequesters excess intracellular iron for storage in the ferric form, with up to 4500 iron atoms stores in each ferritin molecule.
Ferritin levels are the most sensitive and specific marker for iron deficiency in adults and children. Evidence has shown that ferritin is the best test for the diagnosis of iron deficiency in all age groups.
Likelihood Ratios of Iron Deficiency Associated with Different Ferritin Levels
Ferritin should be ordered with a CBC in patients with risk factors for iron deficiency.
In the presence of inflammation, ferritin will be elevated as it’s an acute phase reactant, and in the majority of patients with inflammation, a ferritin level below 100 mcg/L with transferrin saturation below 20% is consistent with iron deficiency and should be replaced. Examples of inflammatory states: Acute and chronic infections Heart failure Chronic kidney disease Autoimmune conditions (e.g., systemic lupus erythematous, rheumatoid arthritis, inflammatory bowel disease, vasculitis, psoriasis) Hematological and solid-organ malignancy Patients with elevated BMI Patient post-transplant
There are certain populations where a higher ferritin threshold is used for diagnosis of iron deficiency:
In patients with heart failure, a ferritin level of <100 μg/L or <300 μg/L with a TSAT <20% is the recommended threshold for diagnosis. (5)
In patients with chronic kidney disease with a normal hemoglobin, iron therapy is warranted if ferritin is ≤100 μg/L and TSAT is ≤20%, but if there a decreased hemoglobin (Hb < 120 μg/L for women, and <130 μg/L for men), iron therapy is indicated if ferritin <500 μg/L and TSAT ≤30%. (6)
Patient Populations with Associated Ferritin Levels
*If adult patients have concomitant inflammation with Ferritin >30, order iron studies (serum iron, TIBC, transferrin saturation). For pediatric patients with concomitant inflammation and Ferritin >20, order iron studies or soluble transferrin receptor. If iron studies are required for patients with inflammation, indicate “chronic inflammation” on the Ontario Ministry of Health lab requisition form in the clinical information section.

Iron Profile
An iron profile will typically show:
Low serum iron
Increased TIBC/Transferrin This test can help differentiate ID from anemia of inflammation (AOI) as it is usually normal/low in AOI.
Low transferrin saturation (TSAT), i.e. less than 20% An overnight fast is recommended before measuring the iron profile, to help increase the sensitivity, as alone, it is not sensitive nor specific for diagnosis of iron deficiency as: Serum iron is also low in anemia of inflammation, and is affected by recent dietary intake or supplementation. TSAT can also be low in AOI due to increased Hepcidin and resulting iron sequestration, with each transferrin molecule able to bind to 2 iron atoms, compared to Ferritin which binds to 5000 iron atoms.

Soluble Transferrin Receptors (sTfR)
sTfR is elevated in iron deficiency and does not rise in inflammatory states, making it a good marker for differentiating from anemia of inflammation. sTfR are markers of bone marrow iron stores and erythropoiesis. Limitations of this test include scarce testing availability and absence of standardized cut-offs worldwide.

Bone Marrow Biopsy
Absence of stainable iron on a bone marrow biopsy is the gold standard for diagnosing iron deficiency as it is not affected by inflammation and is highly specific. However, this test is reserved for specific cases as it is invasive and uncomfortable for the patient.

Investigating the Underlying Etiology
Iron deficiency is the presenting manifestation of various pathologies, and investigations aimed at identifying the possible cause is essential.
The extent and nature of testing depends on the patient demographics and clinical setting. Men and postmenopausal women with iron deficiency at high risk of bleeding gastrointestinal lesions should be considered for both upper and lower gastrointestinal endoscopy. Testing for celiac disease should be considered in individuals with iron deficiency, with measurement of anti-tissue IgA transglutaminase antibodies (tTG-IgA) being the preferred test, and should be combined with IgA concentration, to rule out IgA deficiency.
Identifying the Etiology of Iron Deficiency